Cheryl Chafos honors her late son, Zachary, by advocating for autism training among healthcare professionals
“My son passed away on August 24, 2021. I don’t want Zachary’s life to feel like it was a waste or that he wasn’t here just because he had autism.”
The first thing Cheryl Chafos will tell you about her son Zachary, Zach to those lucky enough to know him, is that he was a very happy person and loved people. Pizza and Chick-fil-A were up there, too. He also happened to be something of a Pixar aficionado, favoring the original Cars and Toy Story movies. He was a real character himself and got a kick out of reenacting those two classics, along with Up and The Incredibles to entertain his three brothers.
His brothers -- one older and two younger. They loved when he wanted “big hugs” or said, “love you more.” And Zach was their biggest fan. He would get upset when Cheryl and his dad, Tim, a retired Army colonel, disciplined them or when anyone tried to correct them. To him, imperfection was perfection.
The beach was Zach’s happy place. He looked forward to the family’s annual summer vacation at their favorite New Jersey shore spot where he soaked up the sun, played in the sand and strolled the boardwalk. But his absolute favorite activity was surfing. He had his first taste in Belmar, NJ, in 2011 through Surfers Healing, a California-based surf camp for kids with autism, and was instantly hooked. Every year after, he looked forward to catching waves with professional surfers for his "One Perfect Day".
Zach was also a 19-year-old nonverbal autistic young adult with intellectual disabilities who suffered from seizures since age 14 and had some challenging behaviors, developing aggression as he got older. While he participated in Special Olympics and was attending Kennedy Krieger High School in Baltimore, MD, Cheryl noted she constantly struggled to keep Zach busy and engaged. A trampoline helped but he thrived being with people and needed community activity.
Then came the pandemic shutdown. Like so many, with and without a disability, Zach struggled being isolated from his normal activities. There was not a trampoline big enough to fill the void he experienced. His aggression increased at home where he was confined most of the time.
In the fall of 2020, the Chafos’ reached a breaking point. Zach’s therapist said he would be best served at Sheppard Pratt, the largest private, nonprofit mental health system in the US located in their home state of Maryland. But the therapist said Zach would have to get there via their local emergency department – the typical road to admission for those who end up at psychiatric hospitals. So when Zach exhibited some severe behavior on November 12, 2020, they went to Howard County General.
The Emergency Medical Treatment and Labor Act (EMTLA) mandates that an emergency room must offer to treat a medical condition until a patient is stable, or if it doesn't have the capability to stabilize the emergency medical condition, it must offer to transfer the patient to a hospital that is capable of treating the emergency medical condition.
Howard County General could do neither for Zach. The ER is for things like broken bones and other severe sudden onset injuries that require immediate care, and its staff trained accordingly. It is not a place for an autistic person experiencing a mental health crisis. But there were no beds at Sheppard Pratt or any psychiatric beds at any hospital anywhere nearby for Zach.
So Zach stayed in a windowless ER room, uncomfortably surrounded by the noises of sick and injured patients coming/going, and only allowed one visitor a day for a limited period of time – for 28 days. That’s 27 days and 20 hours longer than is recommended for an ER stay by the Joint Commission, a nonprofit organization in charge of hospital accreditation.
Zach’s mental health worsened as the days went on and he became aggressive with staff. Those in the autism community know that such behaviors are a result of an autistic person being unable to communicate or express their thoughts, feelings, needs and even their pain in a way that others can understand. But special needs had to take a backseat to ER safety protocol. Zach was frequently restrained and injected with a sedative, haloperidol, which made his body shake so hard he was unable to stably hold a cup and drink from it. A security guard was assigned to his door and he was rarely allowed to leave his room. It was worse than a prison, Cheryl noted. At least prisoners got fresh air and exercise.
On day 29, Zach was finally transferred to Sheppard Pratt where he stayed about two weeks, was medically stabilized and discharged to reunite with his family on Christmas Eve.
Soon after, Zach’s behavior returned, worse than before. His younger brothers were now so scared they often locked themselves in the bathroom. Cheryl and Tim were looking into group homes but none would take him while he exhibited aggressive behavior. But they couldn’t handle him on their own either. So with heavy hearts and no other place to turn, they made the decision on June 28, 2021 to take Zack back to the ER so they could get him back to Sheppard Pratt.
This time Howard County General's ER was overflowing with patients dealing with mental health crisis. One woman near him screamed at all hours; a man nearby was handcuffed to his bed. Two weeks in, a nurse told Cheryl she should stop visiting every day because when she and Tim left, Zach became upset and sometimes violent. The nurse wanted Zach to settle into a routine. It was if she was clairvoyant. Zach would end up waiting seven weeks in the ER, almost twice as long as he did in the fall.
The Washington Post reviewed Zach’s 955-page medical file and found that during his second ER stay he was set off by loud noises, punched staff and pulled their hair, was restrained and sedated, and was unable to respond to hospital staff questions except with lines from Pixar movies. His file notes one thing he did say that was crystal clear: I want to go home.
On day 49 in the ER, Zach was finally transferred to Sheppard Pratt. Cheryl noticed his skin had changed from lack of sunlight, he had bags under his eyes, his hair was disheveled and he walked differently. She was met with one recognizable feature though. When she hugged him, he gave her back one of his “big hugs.”
It would be the last one she ever received. Over the next 9 days she and Tim were only able to video call Zach twice. Then on August 24, while out on the soccer field watching her youngest son practice, Cheryl got the tragic phone call from Sheppard Pratt. Zach had passed away.
For 19 years Cheryl spent countless hours advocating on Zach’s behalf with school staffs, doctors, therapists, support agencies and others-as well as driving to therapies, consultations and events. She had spent the last 59 days up every night wondering if first Howard County General and then Sheppard Pratt were feeding, bathing, taking care of her boy. Wondering if Zach thought his mom abandoned him. Now he was gone. She was numb, in a living nightmare, with a shattered heart and a giant hole in her family.
Zach died from suspected SUDEP, or sudden unexpected death from a seizure; his autopsy report listed seizure.
“The infrastructure that was in place let us all down,” she said. “Nobody really had any solution on how to help Zachary and how to get him stable.”
It has only been about two and a half years since Zach passed away and Cheryl feels pain and sadness every day. But advocacy is one way she says she can contribute, carry on Zach's memory and honor him. This past March she went to Capitol Hill with Autism Speaks to ask congressmen to sign the reauthorization of the Autism CARES Act 2024 into law.
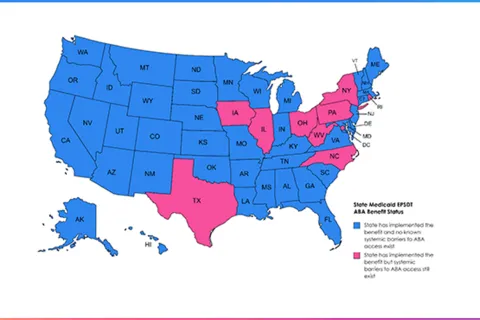
The Autism CARES Act, which originally became law in 2006, is the only piece of federal legislation solely dedicated to improving the lives of autistic people. If the 2024 bill passes, it would authorize over $2 billion in funding over the next five years for programs primarily at the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC), and the Health Resources and Services Administration (HRSA) that advance autism research, services, and training of health care professionals.
Specifically, while the Autism CARES Act has raised awareness and understanding of co-occurring mental health conditions, additional research is needed to better recognize and address mental health issues in those like Zach with challenging behaviors and high support needs. Research and clinical programs supported by Autism CARES Act could help develop more personalized treatment approaches.
“There are a lot of people in our autism community that are struggling, like Zachary was struggling, and feel hopeless and their families feel hopeless because they don’t know what to do,” said Cheryl. “This money could go towards training to help stabilize adults like Zachary so they can live their best lives in the community.”
“Zachary’s life was important. His love for life and his outlook on life was a gift to us all,” said Cheryl. “I need to speak for those who can’t speak for themselves and continue the fight for those like Zachary.”
Learn more:
- CEO’s Letter: Addressing the crisis in access to autism care
- Autism and mental health in young people